Creating Cancerous T-Stem Cells to Aid AIDS Patients
By Hailee Bilimoria
Originally published on February 23, 2018
Cancer cells have always had a very negative connotation, but with proper knowledge and comprehension of the cell cycle, the roles of different cells in the body, and the effects of cancer cells, scientists may be able to harness the power of cancer cells and use them for the common good. Using the benefits of cancer alongside the advantages of t-stem cells, society can revolutionize the medical treatment for AIDS patients worldwide.
T-lymphocytes, also known as t-cells, originate in the bone marrow (National Institute of Health), but mature in the organ known as the thymus, which is why they bear the “t” in their name (Biology Online Dictionary). T-cells one of many different types of cells that come from myeloblasts and lymphoblasts such as b-lymphocytes, natural killer cells, and granulocytes, all of which are white blood cells. White blood cells are types of immune cells in the body (National Institute of Health). T-cells, more specifically, split into divisions of cells with specific duties. For instance, the function of a regulatory t-cell is repress the immune system’s activation, maintain its homeostasis. Suppressor t-cells inhibits immune system responses by sending messages to other white blood cells. Memory t-cells are aged cells that remember defenses used against pathogens that had previously entered the body. Cytotoxic t-cells help kill cancerous cells, and unfortunately, somatic cells if need be. Lastly, the most important of the t-cells, the t-stem cell. T-stem cells are t-cells that have not yet been assigned a function. At this time, the immature cells must migrate to the thymus to mature and become one of the many types of t-cells (Biology Online Dictionary). As fighters of foreign invaders and protectors within the immune system, t-cells are arguably the most important cells in the entire human body.
Image of t-lymphocytes, also known as t-cells, housed in the thymus.
After the G2 checkpoint is confirmed, the cell divides in the second part of the cell cycle: mitosis. In prophase, the first phase of mitosis, the chromosomes within the cell are condensed. In the second phase of mitosis known as metaphase, spindle fibers, a rod shaped structure made of microtubules and different proteins, connect to the centromeres of the chromosomes and guide them in a line in the center of the cell. Before additional phases may proceed, the mitosis checkpoint must be completed. This checkpoint reassures that all the spindle fibers are connected to the centromeres of each chromatid. In the third phase known as anaphase, the spindle fibers pull the sister chromatids apart. Lastly, in telophase, daughter nuclei reform at the two poles of the cell. This happens alongside cytokinesis, which is the division of the cytoplasm into separate daughter cells. For plant cells, a cell wall manifests itself in the cell, while in animal cells, the process is known as cleavage and involves the pinching of the cell into two separate cells. Following cytokinesis, the cell cycle is complete and the cycles of the two daughter cells are just beginning!
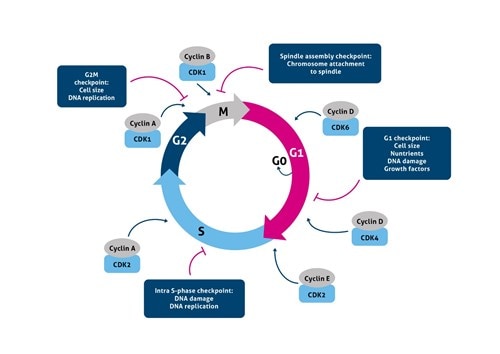
Image of the cell cycle with the regulators used at each point.
Cancer cells are created by a single cell mutating. Through this mutation, they are able to divide rapidly through unchecked growth. The mutation is able to accelerate the rate of cell division and inhibit regulators’ functions. The lack of checkpoints and regulators in turn takes away the cells mortality. As the cell continues to rapidly reproduce without the help of checkpoints and regulators, as previously mentioned, the function of the cell will not be proper. Mutations will continue to form and the original function of the cell will be lost. The malignant cells will continue to multiply and spread to the rest of the body, eventually killing the host (Dyson). The rapid cell division and immortality of cancer cells greatly contribute to the high mortality rate of cancer patients, but in the world of science, the effects of cancer cells can be both a blessing and a curse.
The mutation of cancer cells may be a very somber topic, but there are many potential benefits that can come from its strengths, especially when using cancer cells alongside t-stem cells. If scientists were to take t-stem cells in the early stages of their mutation and insert them in the bone marrow, the host body would be able to get their t-cell count up quite high in a safe way. During t-stem cell maturation, according to the Biology Online Dictionary, “[any] T cells that may potentially act against body's own tissues are destroyed” (Biology Online Dictionary). After the t-stem cells reach the thymus and endure part of their cell maturation, they could be cited as “positively selected” cells, which means they are allowed to fully mature and become specialized t-cells that can also reap the rewards of cancerous cells, such as quick cell division and immortality (Abbas, A. K., & Lichtman, A. H.). These t-stem cells could then distribute themselves into specified t-cells that are needed within the host as they see fit. If any cell were to possibly over-mutate and become potentially dangerous, it would not be able to mature and it would be classified as “negative” (Abbas, A. K., & Lichtman, A. H.). A cell that is within the realm of negative selection would either be terminated or it has a chance to activate its “rescue mechanisms” (Abbas, A. K., & Lichtman, A. H.) The rescue mechanisms include excluding certain alleles, editing the receptors, and even changing the genetic material of the cell itself. Essentially, the cancerous t-stem cell could remove its mutation before maturation while still taking advantage of the cancer’s quick reproductive effects! In summary, this cancer would provide two potential pathways to get t-cells into the body: a malignant, therefore immortal and rapidly reproducing cell would be further specified, or the cancerous cells would remove their mutation and then specify themselves. Either way, creating cancerous t-stem cells provides a profound approach to artificially create more t-cells of all functions.
Image of the process in which t-stem cells go through to decide whether they are within the positive or negative selection realm
Through the use of cancer’s rapid cell division and t-cell’s immune system power, scientists can revolutionize the way that AIDS patients are treated. Acquired Immunodeficiency Syndrome, or AIDS, is the result of the Human Immunodeficiency Virus, or HIV. According to HIV.gov, HIV heavily attacks the immune system and especially t-cells. AIDS is “the most severe phase of HIV infection” (HIV.gov). A person is diagnosed with AIDS when their t-cell count falls below 200 cells per cubic millimeter, while the average healthy person has anywhere 500 to 1600 cells per cubic millimeter (HIV.gov). Through the use of t-stem cell cancer, all types of t-cells, both mortal and immortal, could be recreated and restored in the bodies of AIDS patients with little hindrance from HIV. The use of cancerous t-stem cells is a great way for AIDS patients to have a treatment plan that requires minimal medications and promises real results. While it does not kill the virus, it does help restore the detrimental effects caused by HIV. Because the patients that are using these cells have such a harmful virus and such a serious condition, there is no need to stop the spread of the t-stem cells within the body. There will be a constant need for them, for the t-cells are not completely safe from the virus. However, if it is absolutely necessary to stop the cancer, the introduction of natural killer cells, white blood cells known to kill cancer cells, would help attack the t-cell mutations (Biology Online Dictionary). Through the use of this treatment, AIDS patients could finally have their life back.
The use of cancer cells to reproduce t-stem cells may seem like a risky job, but with knowledge on the different parts on the cell cycle, cell regulators, and cancer cells makes the benefits of cancer cells more and more clear. Hopefully, in the near future, scientists will find a way to harness the power of cancer cells and use them for the common good and make this proposal into a reality.
Footnotes
1 Explain the purpose of the parts of the cell cycle, including mitosis
2 Explain how changes in the cell cycle can affect organisms
References
Abbas, A. K., & Lichtman, A. H. (1991). Stages of Lymphocyte Maturation. In Cellular and Molecular Immunology. Retrieved February 23, 2018, from https://www.uni- salzburg.at/fileadmin/multimedia/Molekulare%20Biologie/documents/AG_Thalhamer/C08_Rea rrangement.pdf
Biology Online Dictionary. (n.d.). T cell. Retrieved February 19, 2018, from https://www.biology- online.org/dictionary/T_cell
Dyson, R. D. (1978). Essentials of cell biology[Scitable by Nature Education]. Boston: Allyn and
Bacon. Retrieved February 23, 2018, from https://www.nature.com/scitable/topicpage/cell-division- and-cancer-14046590.
HIV.gov. (2017, September 26). What Are HIV and AIDS? Retrieved February 19, 2018, from https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/what-are-hiv-and-aids
National Institute of Health. (n.d.). T-Lymphocytes - National Library of Medicine - PubMed Health.
Retrieved February 19, 2018, from https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0022044/
T. Clark Brelje, & Robert L. Sorenson. (n.d.). MH 079 Thymus - Image. Retrieved February 19, 2018, from http://histologyguide.com/slide-view/MH-079-thymus/10-slide-1.html? x=14242&y=27429&z=100&page=1
U.S. Department of Veterans Affairs. (2005, June 21). HIV/AIDS. Retrieved from https://www.hiv.va.gov/patient/diagnosis/labs-CD4-count.asp




Comments
Post a Comment